TMJ refers to the temporomandibular joint, which is the bone structure, muscles and connective tissues that surround the jaw and control chewing. When patients experience disorders of this joint, they are said to have a temporomandibular joint disorder or TMD. Symptoms of TMD include pain and tenderness near the jaw, as well as popping or clicking in the joint when speaking or chewing. There are many ways of treating TMJ disorders, ranging from non-invasive therapy and bite splints to injections or surgery. Left untreated, however, TMJ disorders can lead to headaches, muscle pain, malocclusion and tooth damage from grinding or clenching.
TMD alone is not a disorder, but instead a collection of disorders that affect the temporomandibular joint? It is the second most common pain-causing musculoskeletal condition in the U.S. according to the U.S. National Institute of Dental and Craniofacial Research, as many as 12 percent of Americans may suffer from some type of TMD, with women twice as likely to be affected than men. But despite the prevalence and wide availability of treatment, only one out every three people with TMD fails to seek treatment.
You will first need to be formally examined and diagnosed with TMJ disorder. You dentist will evaluate the extent of the condition and determine what course of treatment is best for you. Usually, the initial approach involves conservative treatments, such as self-care, physical therapy and bite guards. Medications may also be used to relax the jaw or relieve pain. Patients who do not respond to conservative treatments may be considered for surgery or joint injections.
TMJ treatment varies from patient to patient, so your experience may be very different than someone else’s. You’ll probably be asked to adopt certain lifestyle changes to help facilitate rehabilitation in your jaw. For example, you may be asked to avoid sudden jaw movements, such as yelling or yawning. You may also need to begin sleeping on your back and take steps to reduce your stress levels.
Your post-treatment care instructions will vary according to the type of treatment you receive. If you undergo an aggressive treatment, such as surgery, you may be temporarily subject to an all-liquid diet. You’ll also need to apply ice to the face to minimize swelling and also keep the surgical site clean and dry.
Dental veneers – also known as laminates – are used to cosmetically enhance the appearance of one or more teeth. Veneers are very thin, porcelain or resin shells that are customized for a desirable color and shape. They are bonded to the surface of the teeth to reshape broken, misshapen or irregular teeth, as well as provide a solution for discolored teeth that do not respond to traditional whitening treatments. Patients with veneers typically achieve a natural tooth appearance that is well-tolerated by the gums and also resistant to future stains.
Dental veneers are a conservative way of completely making over your smile? In fact, veneers are a go-to cosmetic procedure that has become popular with celebrities who want a brighter and more symmetrical smile. Miley Cyrus, Hilary Duff and Ben Affleck are just some of Hollywood’s elite who have seen a cosmetic dentist for laminates. Fortunately, affordability and accessibility make it easy for anyone to get dental veneers – including patients.
Dental veneers may be right for you if you are looking for an alternative to crowns and caps. Veneers can help you if you have gaps between your teeth or teeth that are broken, chipped, irregularly shaped or misaligned. To find out more about whether dental veneers are right for you, contact a cosmetic dentist to schedule a consultation.
Before dental veneers can be placed on the teeth, the surface of the teeth must be prepared for bonding. After administering a local anesthetic, your dentist will buff away approximately half a millimeter from the surface of the teeth. You’ll then bite into a mold that will be used to form your veneers in a dental lab. When the veneers are ready, you’ll be asked to return to have them fitted, bonded and adjusted for shape and color.
There is no special care required for dental veneers, and normal brushing and flossing can be resumed immediately. Because veneers are usually placed over the course of two appointments, it is normal to experience some sensitivity between the first and second visit when the teeth have been reduced in preparation for bonding
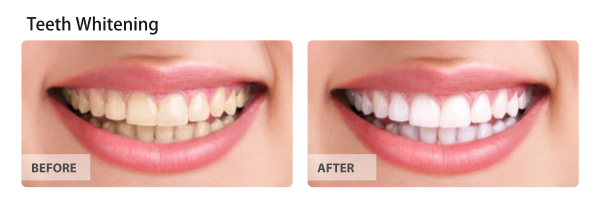
Teeth whitening procedures are used to brighten the appearance of a patient’s smile – sometimes by as many as 5 to 10 shades in a single session. According to the American Dental Association, teeth whitening procedures have become some of the most popular esthetic dental treatments among patients throughout the country, including. Professional teeth whitening services can be performed in an office setting or prescribed for take-home use by a patient. In comparison to over-the-counter teeth whitening treatments, professional whitening uses stronger whitening agents that deliver faster and more effective results.
Teeth naturally darken as we age. Furthermore, certain foods, beverages, medications and habits can contribute to a darker, yellowed, or stained smile. However, it is possible to erase years of stains in a single professional whitening session and sustain those results for many years with proper maintenance. According to the American Academy of Cosmetic Dentistry, professional whitening is best maintained by a combination of good oral care and take-home whitening treatments as recommended by your dentist.
You may be a candidate for professional teeth whitening if you are experiencing discoloration, but otherwise have healthy teeth and healthy gums. Schedule a consultation with a dentist to find out if tooth whitening could be right for you. Some patients, such as those who are pregnant or sensitive to whitening agents, may not be candidates for professional whitening.
Teeth whitening consists of a thorough cleaning and polishing of the teeth, with all debris carefully removed. Your dentist will then protect your gums before applying a whitening agent to the surface of your teeth. The product will be activated and left on the teeth for several minutes before being washed off with water. Your results will vary according to the natural shade of your teeth and degree of discoloration, but it is normal for patients to experience a lightening of several shades in a single visit.
It is normal to experience some tooth sensitivity following a professional whitening treatment. You may be instructed to avoid consuming highly pigmented beverages for at least 24 hours to prevent the teeth from becoming stained again. Examples include tea, coffee and wine. Depending on your results and long-term teeth whitening goals, you may also be sent home from your procedure with an at-home whitening kit for later use.





General dentistry encompasses a broad range of diseases and disorders of the oral and maxillofacial region. Everyone should see a general dentist for routine oral health examinations, twice-yearly cleanings, and treatment of routine oral health complications, such as minor tooth decay. General dentistry is as much about prevention as it is about treatment. Patients who visit a general dentist can expect professional oral health care, as well as education and advisement about self-care between office visits.
Yes. Even if you are not currently experiencing any symptoms of tooth decay or gum disease, it is important to visit your dentist for a thorough examination and cleaning. Despite daily brushing and flossing, your teeth can still accumulate tartar that can harbor bacteria. These bacteria can lead to gum disease and tooth decay if not professionally removed at your dentist’s office.
Based on the results of your dental check-up, your dentist may recommend that you return for treatment or follow a special at-home oral care plan. You may also be referred to a dental specialist for treatment of advanced oral health conditions.
Dental mouth guards have long been used to protect the teeth, gums and supporting tissues from damage, injury and trauma. There are two types of sports mouth guards – over the counter and custom. While OTC guards are helpful for occasional use, many dental patients require the benefit of a customized dental mouth guard fitted by a dentist to effectively prevent injury.
Caring for your new custom mouth guard is simple.
The American Dental Association recommends keeping protected in a sturdy container in between usage. You should also be careful to clean your mouth guard after use and occasionally soak it in cool, soapy water for thorough sanitation. Custom dental mouth guards are designed for durability, but it is important to check your mouth guard for signs of wear every few months. Mouth guards for children and teens must be replaced frequently to account for growing jaws and changes to the teeth.
There are many reasons why wearing a dental mouth guard could be right for you. A few examples include:
Nighttime wear to prevent damage from teeth grinding and bruxism
Tooth and lip protection during high-impact sports, such as martial arts
To serve as a barrier between the lips and oral appliances, such as metal braces
To protect fragile bridgework
Your visit will consist of taking an impression of your teeth that will be used as a mold for your new mouth guard. You may even be able to leave your dental appointment with your custom mouth guard in-hand.
Before you leave your dentist’s office with your new mouth guard, you’ll receive instructions on how and when to wear it. If you suffer from TMJ disorders or bruxism, for example, you will likely wear your mouth guard at night. If you participate in recreational sports, however, you may only need to wear your mouth guard during physical activity.
Tooth extractions are routine dental procedures used to remove decayed, damaged or otherwise problematic teeth. Dentists usually make every effort to preserve natural teeth, although sometimes an extraction is necessary. Although the procedure is performed in a dentist’s or oral surgeon’s office, it is considered surgery. Depending on which teeth are removed, they may be replaced with a dental implant or another oral prosthetic.
There are several reasons why you could need a tooth extraction.
The most common cause of tooth extractions is severe tooth decay and cavities. However, many patients also undergo extractions for impacted teeth – particularly wisdom teeth. Other causes for extraction include advanced periodontal disease, cracked teeth, and teeth that are severely malformed. Although many circumstances that require extraction are unavoidable, some could be prevented with regular visits to the dentist for exams and cleanings.
Only your dentist can tell you if you need a tooth extraction. However, you may be a candidate for the procedure if one or more of your teeth are decayed so severely that a filling or others restoration is not a possibility for treatment.
If you and your dentist decide to extract one or more teeth, you will be scheduled to return for oral surgery at a later date. You will be given a local anesthetic to prevent pain during the procedure, and you may be prescribed medications to help manage pain in the hours following your extraction. Depending on the nature of your extraction and other factors, such as whether your teeth are impacted, you may also be sedated or given general anesthesia during your procedure.
Post-operative care following a tooth extraction is essential for healing and preventing complications. You will be instructed to avoid certain foods and also keep the surgical site clean at all times. If you are prescribed an antibiotic, it is important that you complete the course of treatment to prevent infection. Finally, you may be advised to avoid smoking or drinking through a straw, as doing so may delay the healing process and cause a condition known as ‘dry socket.’
Composite fillings – also known as tooth-colored fillings – are dental restorations designed to be inconspicuous and natural in appearance. They blend well with the teeth and appear more natural than amalgam fillings, which are darker and more easily seen by other people. Composite fillings are made of ceramic and plastic compounds that chemically bond to the teeth. They can be used to fill in decayed areas of the teeth, as well as to help repair chipped or broken teeth. Most dentists use composite restorations to treat the teeth closest to the front of the mouth, as they are more noticeable when patients smile. However, advancements in dental technology and the composition of composite fillings have made it possible for dentists to also use tooth-colored fillings on molars, which receive more wear than other teeth.
Composite fillings allow dentists to preserve more of the natural tooth structure? This is because composite materials chemically bond to the surface of the tooth like an adhesive. The process takes slightly longer to complete than traditional amalgam fillings, but patients can preserve more of the natural portion of the teeth while enjoying a restoration that is discreet and understated.
If you have a cavity, broken tooth, or a deteriorated filling, you may be a candidate for a tooth-colored filling. Schedule a dental consultation to find out if composites are right for you.
During your visit, your gums and teeth will be anesthetized with a local anesthetic near the site of the filling. Once the area is numb, the decayed or damaged portion of your teeth will be removed to make room for the new tooth-colored filling. A resin will be placed over the area and cured with a hand-held light for less than a minute. The new filling will then be shaped and polished before the procedure is complete.
Composite fillings are cured with light at your dentist’s office. You should be able to return to normal activity and oral care immediately after your visit. It’s normal for treated teeth to experience some sensitivity to hot and cold in the days following treatment, but sensitivity that persists beyond a week should be reported to your dentist.
Did you know…
the American Dental Association does not lean toward one type of brush over the other? It does, however, acknowledge that people with upper body mobility restrictions may better benefit from an electric toothbrush instead of a manual brush. Regardless of which type you decide is right for you, the ADA recommends that all brushes be soft-bristled so as to avoid abrasions that can lead to decay and receding gum lines.
Flossing is an important part of an oral hygiene routine, but research suggests that fewer than half of Americans do so daily. Flossing is simple and only takes an extra couple of minutes per day. Developing a healthy habit of flossing can prevent tooth decay and gum disease, and it may allow you to keep more of your natural teeth as you age. So what is the most effective means of flossing?
Need some extra tips?
The American Dental Association recommends using a strand of floss approximately 18 inches in length. It is important to only use clean floss as you move between the teeth. One of the easiest ways of doing this is by looping each end of the floss around your fingers and beginning to floss with the area closest to one end. If you have never flossed, be sure to ask your dentist for a quick in-person tutorial at your next check-up.
Yes. The ADA recommends that everyone floss in order to prevent tooth decay and gum disease. Even if you have restorations, such as crowns or veneers, good oral hygiene is essential for prolonging their use and maintaining your oral health.
You may not experience immediate results from flossing, but over time, your habit will pay off. Flossing can prevent tooth decay, gum disease and tooth loss – all of which can be highly inconvenient and expensive to treat. A piece of floss that costs just pennies could save you thousands of dollars later on.
Yes. In addition to flossing, you should be adopting proper brushing techniques and visiting your dentist at least twice per year for examinations and professional dental cleanings.